Lichen Planus Lichen planus is an itchy skin disease that can last for years, affecting mainly the skin surface and mucous membranes (such as the oral and genital mucosa), less commonly the nails and hair. Lichen planus is not a form of cancer. It is not an infectious disease and is not contagious.
Why does lichen planus develop?
The cause of lichen planus is not known exactly. It is thought to develop as a result of a malfunction of the immune system. The main factors blamed for this condition are hepatitis-C infection, an inflammation of the liver, certain vaccines and medications, and materials used in dentistry such as amalgam (mercury) fillings.
Who develops lichen planus?
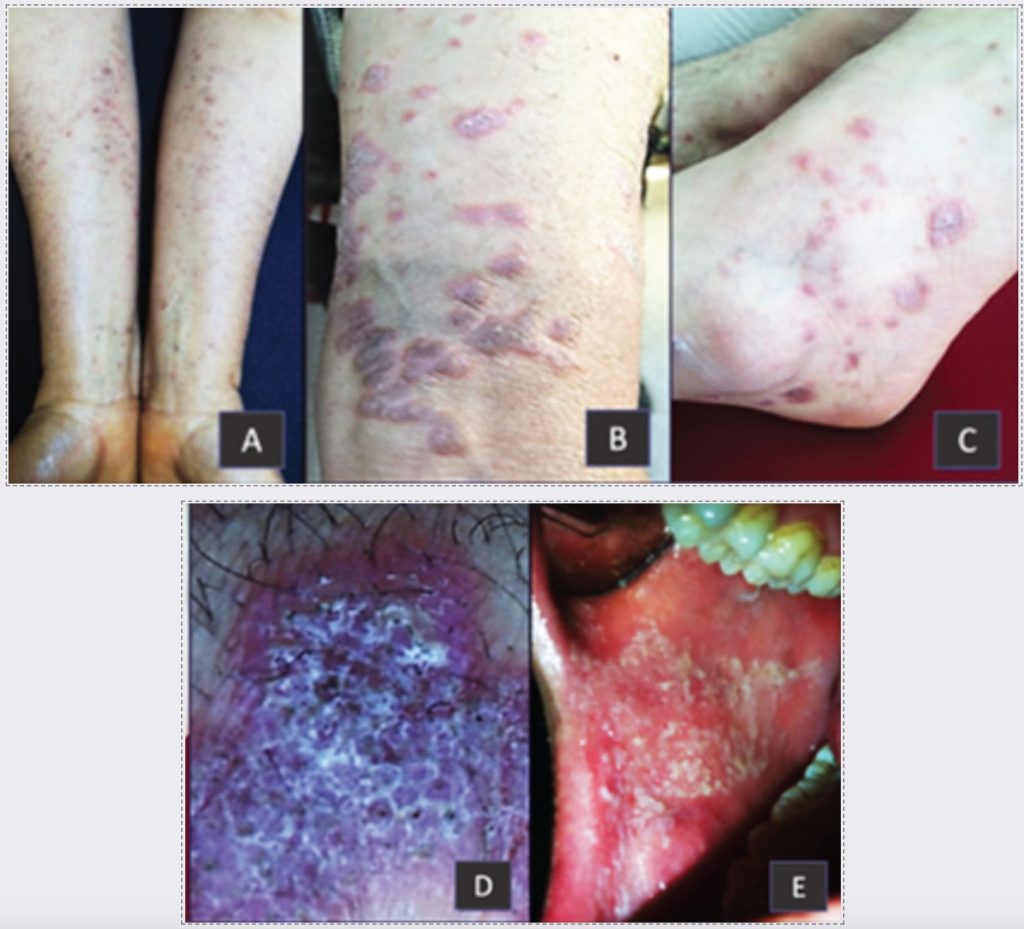
Lichen planus usually occurs in adults over the age of 40. It occurs equally in men and women. Approximately one in every 100 people in the society develops lichen planus. What are the symptoms of lichen planus? Lichen planus is characterized by itchy, purple-pink colored, 3-5mm sized, numerous small raised formations on the skin (Figure 1.A-C). On these small ridges, there are fine white lines in the shape of a net (Figure 1.D). Small wheals may coalesce to form large plaques or ring lesions over larger areas. Although the skin lesions can be located anywhere on the body, usually symmetrically, the most common sites are the inner sides of the wrists and ankles. The disease may involve mucous membranes, mainly oral and genital, and more rarely scalp and nails (Figure 1.E). It is typical for new linear lesions to develop in areas where the skin is rubbed, abraded or scratched. Therefore, the skin of patients with lichen planus should be protected from trauma.
What is the significance of hair, nail and mucous membrane lesions?
Lichen planus lesions can cause itching and disfigurement and may leave long-lasting spots on the skin as they heal. The disease is damaging when it affects the nails and hair; it can cause permanent hair loss in the form of nail deformities and patches on the scalp. This condition develops as a result of delayed treatment, especially in patients who present late to the dermatologist. Mucosal lichen planus lesions pose a risk for the development of oral and genital mucosal cancers in patients.
How is lichen planus diagnosed?
Lichen planus lesions are easy to recognize on examination by a dermatologist. However, a skin/mucous membrane biopsy and histopathologic examination is necessary for the definitive diagnosis of the disease. Discontinuation of local and systemic treatments (especially those containing cortisone and similar) before the biopsy procedure (on average 1 week before) will ensure that the biopsy material will give more accurate results under the microscope. For this reason, inform your doctor about any medication you are taking before the biopsy procedure. Biopsy is a simple surgical procedure that is usually performed by appointment in an outpatient clinic using local numbing needles. Keep your biopsy report carefully to facilitate the follow-up of your disease. How does the disease progress? Lichen planus usually lasts for several years and is characterized by attacks. More rarely, it can be lifelong; its appearance, distribution and treatment requirements may vary during the course of the disease. Rarely, it may progressively involve mucous membranes such as the esophagus and eyes. Discontinuation of medications that may cause lichen planus (especially medications for high blood pressure, heart diseases, malaria and rheumatism) or group group group changes can contribute to the regression of the disease.
How is the disease treated?
There is no definitive treatment that completely eliminates lichen planus disease. However, the main goal in the treatment of lichen planus, which is highly itchy, is to relieve itching and to improve the clinical appearance of the patient until the disease ends. There is no uniform treatment protocol since the type of involvement of the disease varies from patient to patient. Lichen planus treatment must be planned by a dermatologist. What kind of medications are used? The most commonly used drugs in the treatment of lichen planus are local corticosteroid (cortisone) drugs and anti-itch tablets. In severe disease, immunomodulators such as corticosteroid tablets, vitamin A derivatives and ultraviolet light treatments are used. Skin care, avoiding trauma and follow-up are important in lichen planus, which is a long-term disease. Do not go beyond the recommendations of your dermatologist, use your medications regularly, and do not neglect your doctor's visits.

